
Depression Therapy

Depression Therapy
Understanding Depression: Causes, Symptoms, and Treatment
Depression is a complex mental health condition that affects millions of people worldwide. It goes beyond temporary sadness and can significantly impact daily life, relationships, and overall well-being. Understanding depression, its causes, symptoms, and treatment options is essential for those experiencing it and their loved ones.
What is Depression?
Depression, also known as major depressive disorder (MDD), is a mood disorder characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in daily activities. It can affect how a person thinks, feels, and behaves, leading to emotional and physical problems.
While everyone experiences sadness at times, depression is more than just feeling down. It is a prolonged condition that can interfere with work, school, relationships, and overall quality of life.

Causes of Depression
Depression does not have a single cause. Instead, it results from a combination of biological, psychological, and environmental factors. Some common causes include:
Biological Factors
Hormonal Changes: Hormonal fluctuations, such as those occurring during pregnancy, menopause, or thyroid disorders, can trigger depression.
Genetics: A family history of depression can increase the risk of developing the condition.
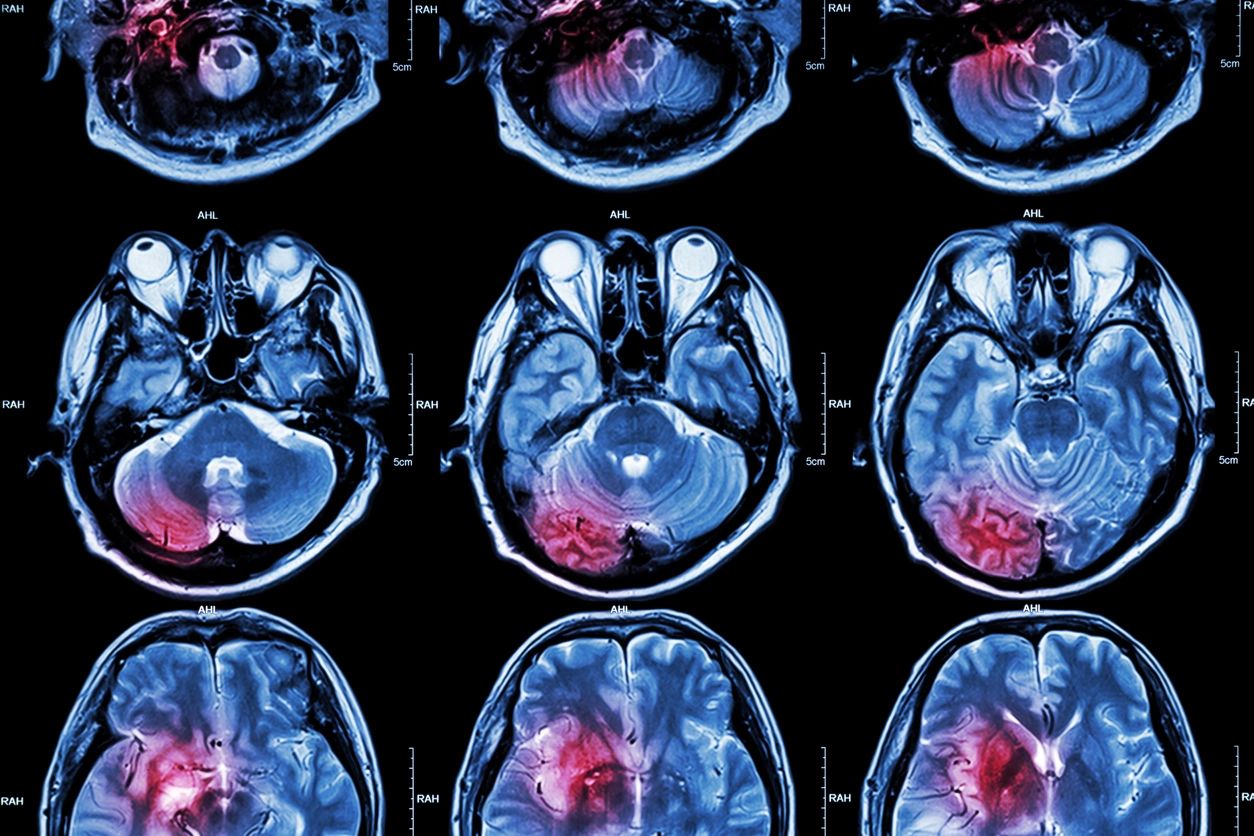
Brain Chemistry: Imbalances in neurotransmitters such as serotonin, dopamine, and norepinephrine can contribute to depressive symptoms.
. Psychological Factors
- Personality Traits: Individuals with low self-esteem, perfectionism, or a tendency to be overly self-critical may be more prone to depression.
- Past Trauma: Childhood abuse, neglect, or other traumatic experiences can increase vulnerability to depression.
3. Environmental Factors
Substance Abuse: Alcohol and drug use can lead to or exacerbate depression.
Stressful Life Events: Loss of a loved one, financial difficulties, divorce, or job loss can contribute to depression.
Social Isolation: Lack of social support and loneliness can worsen depressive symptoms.


Physical Symptoms
- Fatigue or low energy
- Changes in appetite (overeating or loss of appetite)
- Sleep disturbances (insomnia or excessive sleeping)
- Unexplained aches and pains
Behavioral Symptoms
- Withdrawal from social activities
- Neglecting responsibilities at work or home
- Increased substance use
- Suicidal thoughts or behaviors
If you or someone you know is experiencing suicidal thoughts, seek immediate help from a mental health professional or crisis hotline 988.
Types of Depression
Depression can take different forms, including:
1. Major Depressive Disorder (MDD)
Characterized by severe symptoms that interfere with daily life and last for at least two weeks.
2. Persistent Depressive Disorder (Dysthymia)
A chronic form of depression lasting for two years or more, with symptoms that may be less severe but persistent.
3. Bipolar Disorder
Involves episodes of depression alternating with periods of mania or hypomania.
4. Seasonal Affective Disorder (SAD)
Depression that occurs during specific seasons, typically in winter, due to reduced sunlight exposure.
5. Postpartum Depression
A type of depression that affects new mothers after childbirth, often due to hormonal changes and stress.


Treatment Options for Depression
Depression is treatable, and various approaches can help individuals manage their symptoms and improve their quality of life.
1. Therapy
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and change negative thought patterns.
- Psychodynamic Therapy: Explores past experiences and emotions to address underlying issues.
- Interpersonal Therapy (IPT): Focuses on improving relationships and communication skills.
2. Medication
- Antidepressants: Medications such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) can help balance brain chemistry.
- Mood Stabilizers: Used for individuals with bipolar disorder to manage mood swings.
3. Lifestyle Changes
- Regular Exercise: Physical activity boosts mood and reduces stress.
- Healthy Diet: Nutrient-rich foods support brain function and overall well-being.
- Adequate Sleep: Maintaining a consistent sleep schedule can improve mood and energy levels.
4. Support Systems
Mindfulness and Meditation: Techniques such as deep breathing and meditation can help manage stress.
Social Support: Connecting with friends, family, or support groups can provide emotional encouragement.
Coping Strategies for Depression
In addition to professional treatment, individuals can adopt coping strategies to manage their symptoms:
Seek Help When Needed: Reaching out to a therapist or counselor can provide valuable support.
Set Realistic Goals: Break tasks into smaller steps to avoid feeling overwhelmed.
Engage in Enjoyable Activities: Hobbies and creative outlets can provide a sense of fulfillment.
Practice Self-Compassion: Avoid self-criticism and acknowledge progress.
Limit Alcohol and Drug Use: Substance use can worsen depressive symptoms.


Conclusion
Depression is a serious but treatable condition. Understanding its causes, symptoms, and treatment options can empower individuals to seek help and improve their mental health. If you or someone you know is struggling with depression, reaching out to a mental health professional can be a crucial step toward recovery.

Coming Soon!